Audiology covers not only hearing but also the balance system, so a comprehensive evaluation answers two questions at once: “Why has my hearing sensitivity worsened?” and “Why do I sometimes feel dizzy?”. In addition to conventional pure-tone audiometry, modern clinics increasingly add high-frequency screening (8–16 kHz)—the very range where hearing typically “drops off” first, long before everyday conversation becomes difficult. Early detection allows preventive steps: custom earplugs for musicians, switching off ototoxic medications, or equalizing middle-ear pressure. The cost of a standard test is comparable to a massage session, but its value is priceless: your audiogram becomes a “map” of your hearing that lets professionals track even the smallest year-to-year changes.
Warning Signs That Signal a Visit to the Audiologist
Mild hearing fatigue often masquerades as simple irritability: a person loses focus faster, mishears instructions, and starts avoiding phone calls. Meanwhile, the brain works overtime to decode speech, leading to evening migraines and a desire to “turn off the world’s sound”. At this stage it is crucial to spot the red flags and get checked if any of these symptoms look familiar:
- frequently turning up the TV or phone volume,
- difficulty understanding speech in a noisy restaurant,
- ringing or “ocean” sounds in the ears,
- feeling that people mumble and asking them to repeat,
- dizziness or balance problems.
Even one item on this list persisting for more than a month is a reason to schedule an appointment. After a full audiological work-up at North Fulton Ear Nose & Throat, you’ll receive a detailed explanation of the results and clear recommendations to prevent further hearing loss.
Risk Groups That Should Have Regular Audiology
Certain jobs and medical conditions greatly increase the chance of hearing damage. In the U.S., employees exposed to noise above 85 dB every day get an annual test paid for by OSHA. The earlier an audiogram records the “first dip”, the cheaper and simpler it is to treat, because modern hearing aids are nearly invisible and sync with smartphones. Those who should never skip the audiologist include:
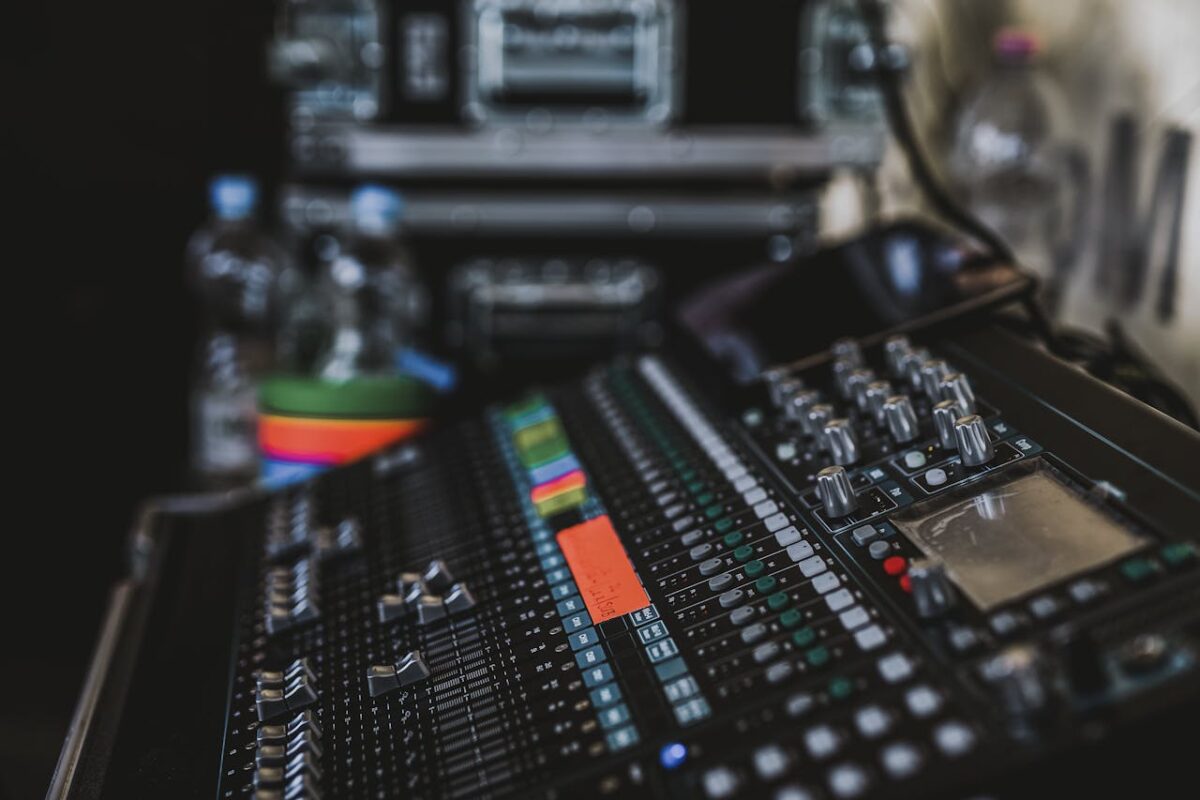
- Musicians, airport workers, construction and industrial staff exposed to > 80 dB.
- Children with three or more ear infections a year or speech delays.
- People with diabetes, hypertension, or autoimmune diseases.
- Patients taking ototoxic drugs (furosemide, aminoglycosides, etc.).
- Anyone over 60, especially with a family history of age-related deafness.
After testing, the audiologist will explain which headphones and noise-reduction settings suit you, whether to add magnesium and B-vitamins to your diet, and how to “rest” your ears after loud shifts. Timely correction of even moderate loss lowers the risk of cognitive decline and social isolation later in life.
What to Do If the Exam Finds a Problem
Don’t panic—and don’t delay the next step. The auditory system is like a muscle: without stimulation, neural pathways atrophy in 18–24 months. If your audiogram shows early sensorineural hearing loss, you should:
- Begin auditory rehabilitation—speech-discrimination drills and “central hearing” training.
- Choose a hearing aid or in-canal amplifier that boosts only the needed frequencies.
- Review medications with your primary-care doctor and replace ototoxic ones.
- Limit noise exposure: quality earplugs, noise-canceling headphones, “quiet breaks” every two hours.
Following these steps keeps a constant audio signal to the brain, preserves speech understanding, and improves life quality. With early intervention, most patients return to comfortable communication and dramatically slow progression.
How the Evaluation Works and What Comes Next
The standard protocol includes otoscopy, pure-tone and speech audiometry, and, when needed, tympanometry and otoacoustic emissions. The device draws the graph automatically, but the doctor explains what every curve means. If the loss is conductive, removing earwax, straightening a deviated septum, or placing a tympanostomy tube may be enough. For sensorineural loss, hearing aids or a cochlear implant are offered; today’s devices are smartphone-ready and almost invisible. Remember: auditory-nerve neurons atrophy without input after 18–24 months, so postponing only worsens the outlook. Regular audiology safeguards communication, career, and cognitive health—a smart investment that is hard to overestimate.